“There’s a lot of interest these days in novel local and systemic treatments of noninfectious uveitis,” observes Dilraj Grewal, MD, an associate professor of ophthalmology at the Duke Eye Center in Durham, North Carolina, and associate director of the Duke Reading Center. During a presentation at the Retina World Congress in Fort Lauderdale, Florida, Dr. Grewal reviewed several investigational therapies currently in late-stage clinical trials that may soon expand the treatment armamentarium for noninfectious uveitis.
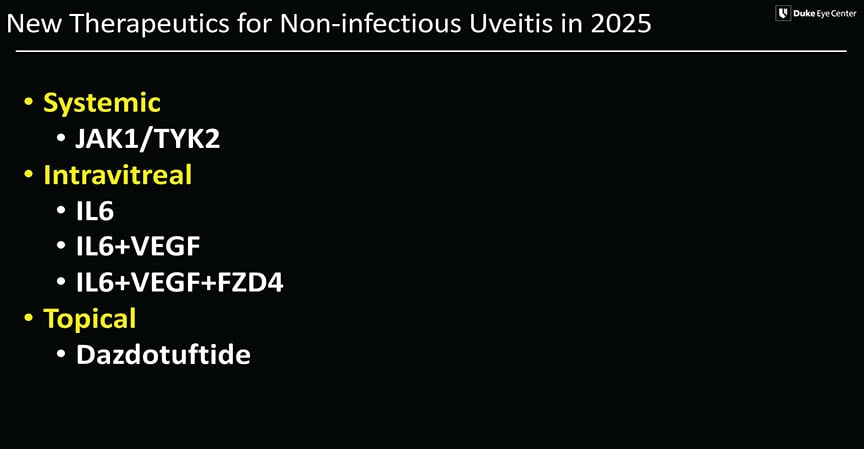
Figure 1. Investigational uveitis therapies for 2025 target multiple mechanisms of action.
One promising systemic treatment is brepocitinib (Priovant Therapeutics), a TYK2/JAK1 inhibitor that targets the inflammatory cascade. The medication is dosed orally once per day. In the phase 2 NEPTUNE study, completed last fall, brepocitinib showed a dose-dependent reduction in inflammation, said Dr. Grewal. That data supported the launch of the phase 3 CLARITY program, which is enrolling 300 participants across 2 substudies in the United States, Europe, Asia, Australia, and South America. Patients will be randomized to receive 45 mg of brepocitinib or placebo, with the primary endpoint being time to treatment failure.
“This is one of the largest programs that is going to look at systemic treatment for noninfectious uveitis,” he said. “It is a placebo-controlled trial, but after 6 months patients will be switched over to the active drug arm. The oral formulation and once-daily dosing makes it an exciting potential systemic therapy.”
Several local therapies are also being studied, with a focus on inhibiting Interleukin-6 (IL-6), a proinflammatory cytokine that contributes to ocular inflammation. Vamikibart (Genentech/Roche) is an IL-6 inhibitor being studied as a treatment for uveitic macular edema that is delivered via intravitreal injection. In the phase 1 DOVETAIL trial, vamikibart demonstrated a favorable safety profile and preliminary efficacy, supporting its progression to the ongoing global phase 3 MEERKAT and SANDCAT trials. “We should be expecting the top-line results this summer,” said Dr. Grewal. “Vamikibart is a very exciting program because it offers the ability to administer local therapy for controlling uveitic macular edema without the side effects associated with local steroids, ie, intraocular pressure elevation and cataract formation.”
Another intravitreal therapy is KSI-101 (Kodiak Sciences), which is being tested in the phase 1b APEX trial for uveitic macular edema. “This is an IL-6 inhibitor combined with a VEGF trap, so it basically gives us the anti-inflammatory effect of IL-6 as well as the antiangiogenic effect of VEGF, which we are all familiar with,” explained Dr. Grewal. “The addition of VEGF trap may allow for a longer durability of effect.” Kodiak plans to initiate 2 pivotal phase 2/3 studies, PEAK and PINNACLE, later in 2025.
SZN-8143 (Surrozen) is an investigational trispecific antibody that combines IL-6 and VEGF antagonism with FZD4 agonism to activate Wnt signaling, regulating normal retinal vessel regrowth and inhibiting pathological angiogenesis. “This is at the moment based on preclinical data, it has not yet entered the phase 1 clinical trials to date,” said Dr. Grewal. “But that is the intent, as intravitreal delivery.”
Finally, Dr. Grewal discussed a topical eye drop formulation of dazdotuftide (TRS01; Tarsier Pharma). TRS01 is a peptide conjugate that includes tuftsin, a natural immunomodulator, and phosphorylcholine. “Phosphorylcholine is actually released by parasites to modulate the host immune system. That’s how this was originally discovered,” he explained. “The TRS01 molecule works by helping to shift the macrophages from the M1 state, which is proinflammatory, to an M2 state, which is anti-inflammatory.”
TRS01 is currently being evaluated in a phase 3 trial against prednisolone acetate for noninfectious anterior uveitis, including eyes with uveitic glaucoma. “The initial results are encouraging, with about 50% of individuals reaching a grade of 0 anterior chamber inflammation and a good safety profile,” said Dr. Grewal. “It gives you the anti-inflammatory effect for anterior uveitis without the associated increase in intraocular pressure.”
During his presentation, Dr. Grewal also provided an update on several once-promising therapies that have failed to advance from clinical trials in 2025. These include the IL-17A inhibitor izokibep (Acelyrin), which did not meet primary or secondary endpoints in a phase 2b/3 uveitis trial that was terminated earlier this year. Evaluation of ESK-01 (Alumis Inc), an oral TYK2 inhibitor that was being studied in the phase 2 OPTYK-1study, was terminated in the fall of 2024 based on interim efficacy data. RP